MUTATED HEREDITY
BRCA1 and BRCA2 are human genes that belong to a class of genes known as tumor suppressors. Mutation of these genes has been linked to hereditary breast and ovarian cancer.
A woman’s risk of developing breast and/or ovarian cancer is greatly increased if she inherits a deleterious (harmful) BRCA1 or BRCA2 mutation. Men with these mutations also have an increased risk of breast cancer. Both men and women who have harmful BRCA1 or BRCA2 mutations may be at increased risk of other cancers.
Genetic tests are available to check for BRCA1 and BRCA2 mutations. A blood sample is required for these tests, and genetic counseling is recommended before and after the tests.
If a harmful BRCA1 or BRCA2 mutation is found, several options are available to help a person manage their cancer risk.
source: national cancer Institute
DON’T NAME NO CANCER AFTER ME!
HER2-positive breast cancer is a breast cancer that tests positive for a protein called human epidermal growth factor receptor 2 (HER2), which promotes the growth of cancer cells. In about 1 of every 5 breast cancers, the cancer cells make an excess of HER2 due to a gene mutation. This gene mutation and the elevated levels of HER2 that it causes can occur in many types of cancer — not only breast cancer. This is a gene mutation that occurs only in the cancer cells and is not a type of mutation that you can inherit from a parent.
HER2-positive breast cancers tend to be more aggressive than other types of breast cancer. They’re also less responsive to hormone treatment.
Women with HER2 positive metastatic breast cancer whose cancer grows despite other standard therapies have a new treatment option available. (see WITH A BULLET)
source: mayo clinic online
WITH A BULLET…
A new ‘magic bullet’ drug called ado-trastuzumab emtansine was approved by the FDA and is giving hope to thousands of women suffering from one of the most deadly forms of breast cancer, HER2-positive. The FDA’s decision was announced in a Feb. 22 news release by the medicine’s developer, Genentech, a member of pharmecutical giant the Roche Group.
The medicine, aimed at an aggressive form of the disease, is expected to offer several months of quality ‘extra’ life and drastically cuts the debilitating side effects of traditional therapy.
In earlier trials, patients found that remission time was on average five months longer when given the drug as ‘first-line’ treatment at an early stage of the incurable advanced HER2-positive form of the disease.
There are also fewer side effects with the drug. Fewer than five per cent of the women given T-DM1 in the earlier study lost their hair, compared with 65 per cent in the control group using traditional chemotherapy.
Other side effects such as diarrhea were also reduced. And half as many of the most serious side effects, requiring hospitalisation, were reported among those given the drug.
T-DM1 teams up the Herceptin antibody with a powerful chemotherapy agent DM1. The two are fused in a way that is more effective.
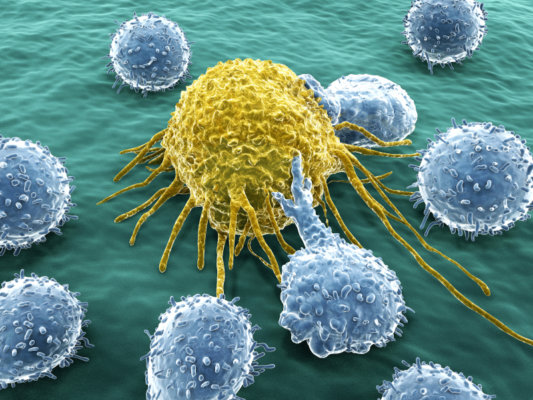
The new drug combination seeks out and attaches itself to cancerous cells, switching off the growth signals that encourage cancer to spread, while calling on the body’s immune system to attack and remove it. The drug then penetrates the cell’s outer layer and delivers the chemotherapy directly inside the cell to destroy it from within.
After the FDA approval, Genentech changed the medicine’s name from trastuzumab emtansine to ado-trastuzumab emtansine to avoid potential confusion, since both Kadcyla and Herceptin’s generic names begin with trastuzumab, a company spokesperson said.
source: daily mail online and living beyond breast cancer
A LIGHTER NOTE: “FOR MEDICINAL PURPOSES ONLY”
DOING THIS:
WILL GET YOU THIS:
Researchers at the UC Berkeley and the Lawrence Berkeley National Laboratory have put the squeeze — literally — on malignant mammary cells to guide them back into a normal growth pattern.
The findings, presented Dec. 17, 2012 at the annual meeting of the American Society for Cell Biology in San Francisco, show for the first time that mechanical forces alone can revert and stop the out-of-control growth of cancer cells. This change happens even though the genetic mutations responsible for malignancy remain, setting up a nature-versus-nurture battle in determining a cell’s fate.
“We are showing that tissue organization is sensitive to mechanical inputs from the environment at the beginning stages of growth and development,” said principal investigator Daniel Fletcher, professor of bioengineering at Berkeley and faculty scientist at the Berkeley Lab. “An early signal, in the form of compression, appears to get these malignant cells back on the right track.”
source: news center berkley edu.